Although a leg ulcer is a wound that shows no signs of improving in 2 weeks, the main reason for it being there needs to be identified by a trained health care professional (nurse or GP).
This may be carried out at the GP practice or by the community nursing service, who may visit you at home.
You will need to have a wound and leg ulcer assessment and this will probably be carried out by a nurse rather than a doctor as nurses are generally responsible for patients with leg ulcers.
This is nothing to worry about and mainly involves questions about your health, medication, symptoms and how long you have had problems with your leg(s).
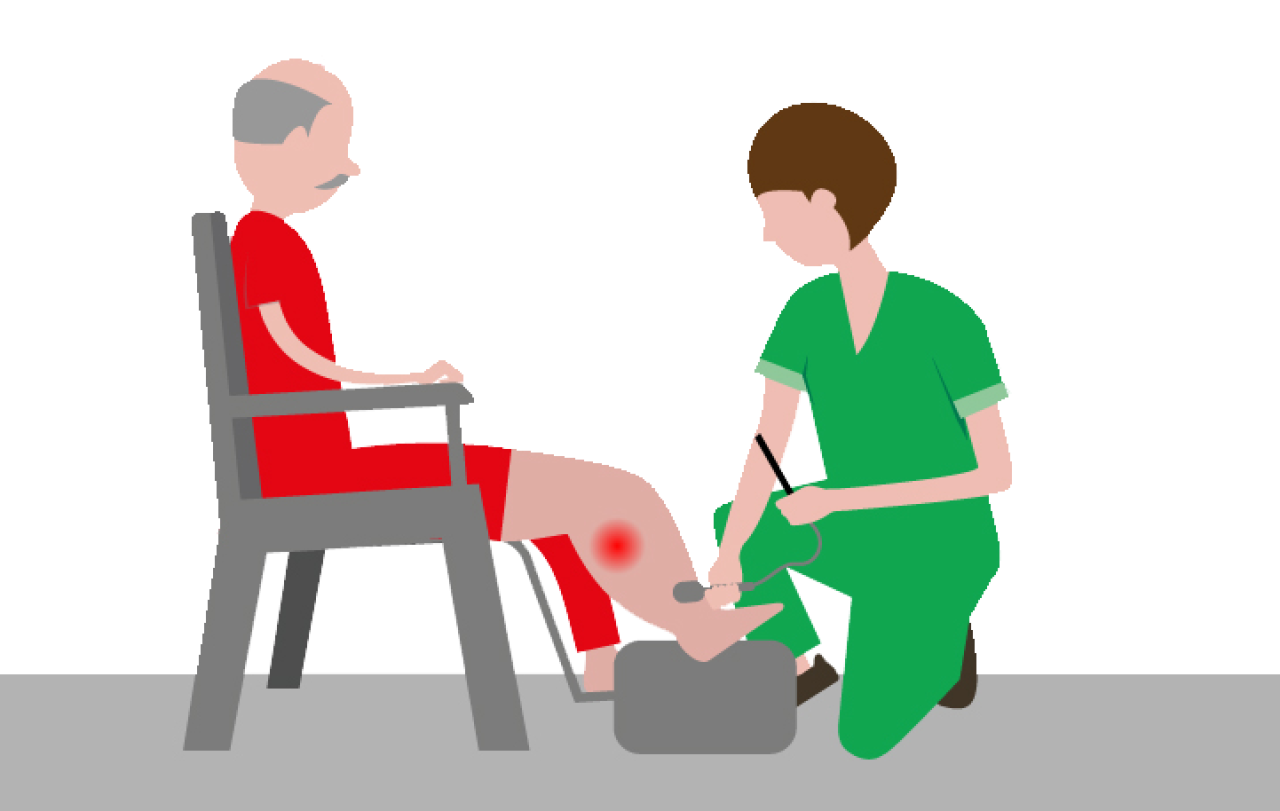
To assess your circulation they will need to carry out a test called an Ankle Brachial Pressure Index (ABPI). This is similar to a normal blood pressure test but compares the blood flow in your arms and in your ankle to see if you have any blood flow problems in your legs.
You may also be asked to have some additional tests for things that can affect healing such as diabetes and anaemia. This is nothing to worry about, it just gives the nurse a better understanding of how they can help you.
What treatment will I need?
The first part of your treatment involves skin care and hygiene. The nurse will want to wash your leg and foot in warm water using a soap substitute to remove any debris or dead skin from the leg and ulcer. Most patients find this part of the treatment process relaxing, calming and gives you a sense of feeling clean. Many of my patients sit and have a cup of tea whilst this is done and leave their leg in warm water whilst I prepare the next part of treatment.
Once your leg and ulcer have been cleaned and dried, the nurse will hydrate your leg using a simple cream, which will minimise itching and prevent your leg from drying out. The ulcer will be dressed in a similar way to any other wound, normally using a simple non-sticky dressing that will need to be changed once or twice a week.
In addition to the dressing, most leg ulcers will be treated using a treatment called compression therapy. This may include a combination of bandages, stockings, socks and wrap around sleeves as your ulcer and leg condition improves. In principle they all do a similar thing. However, as your ulcer gets better there are options that allow you to have more independence and carry out normal activities such as showering.

How is a leg ulcer diagnosed?
If you are able to self care you may be asked to do parts of your treatment at home. Together with clinician, Alison Schofield, we have created a self care series with step-by-step videos to support you to safely wash your limb and surrounding skin, apply dressings and compression socks or wraps. To watch the series visit our YouTube channel.
Wearing compression has proven to help blood flow back to the heart, reduce swelling in your leg, reduce pain and discomfort, reduce itching and dry skin and ultimately help your ulcer to heal.
Find out more about what a leg ulcer is, the causes, advice and treatments.
Find out more about how compression works.

How is a leg ulcer diagnosed?
This blog post has been written by Director of Lower Limb Consultancy Services Ltd, and Honorary Tissue Viability Clinical Nurse Specialist, Sandwell and West Birmingham Hospitals NHS Trust, Andy Kerr.
If you think you may be experiencing leg and foot problems please speak to your GP or nurse as soon as possible.